Understanding Diabetic Retinopathy: Causes & Symptoms
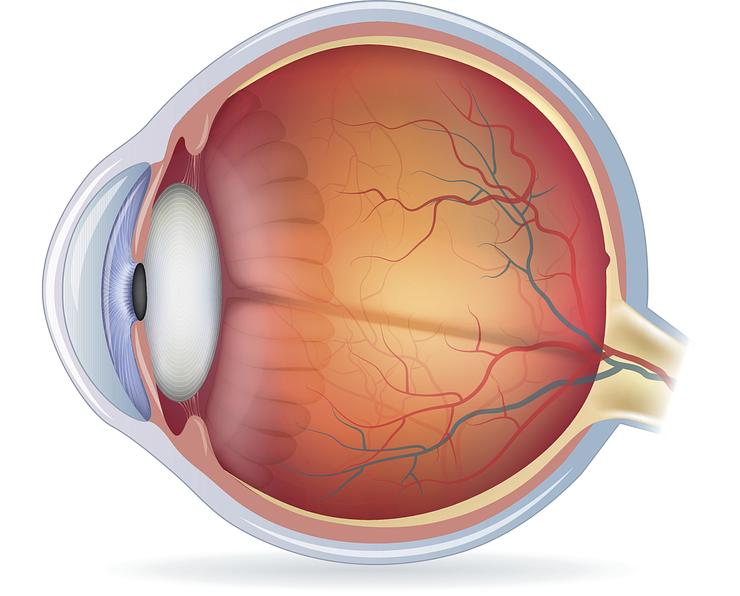
Diabetic retinopathy is a serious eye condition that affects millions of people with diabetes worldwide. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. Left untreated, diabetic retinopathy can lead to vision loss and even blindness. Understanding the causes and symptoms of this condition is crucial for early detection and effective management.
What is Diabetic Retinopathy?
Diabetic retinopathy is a complication of diabetes that occurs when prolonged high blood sugar levels cause damage to the tiny blood vessels in the retina. These blood vessels can swell, leak, or become blocked, leading to a range of vision problems. In some cases, new abnormal blood vessels may grow on the surface of the retina, further compromising vision.
The retina plays a vital role in vision by converting light into electrical signals that are sent to the brain for interpretation. When diabetic retinopathy affects the retina, it can cause:
- Blurred or distorted vision
- Dark or empty areas in your vision
- Difficulty seeing colors
- Vision loss
Diabetic retinopathy can affect both eyes and often progresses without noticeable symptoms in the early stages. This is why regular comprehensive dilated eye exams are essential for people with diabetes to detect and manage the condition before it leads to significant vision impairment.
Why Does Diabetic Retinopathy Occur?
Prolonged high blood sugar levels are the primary culprit behind diabetic retinopathy. When blood sugar remains elevated for an extended period, it can damage the tiny blood vessels in the retina. These delicate vessels become weakened, causing them to leak, swell, or become blocked. As a result, the retina is deprived of the oxygen and nutrients it needs to function correctly, leading to vision problems.
In addition to high blood sugar, other factors can contribute to the development and progression of diabetic retinopathy:
- High Blood Pressure: Hypertension can further damage the already weakened blood vessels in the retina, exacerbating the effects of diabetic retinopathy.
- High Cholesterol: Elevated cholesterol levels can lead to the buildup of fatty deposits in the blood vessels, restricting blood flow to the retina and increasing the risk of diabetic retinopathy.
Did You Know? The longer you have diabetes, the higher your risk of developing diabetic retinopathy. That's why it's crucial to maintain good blood sugar control and attend regular eye exams, even if you don't notice any vision changes.
How to Recognize Symptoms of Diabetic Retinopathy
In the early stages of diabetic retinopathy, you may not experience any noticeable symptoms. This is why regular comprehensive dilated eye exams are so important for people with diabetes. However, as the condition progresses, you may start to notice some changes in your vision:
- Mild Vision Problems: You may experience blurred, distorted, or double vision, which can come and go.
- Floaters: These are small spots, specks, or strings that seem to float across your field of vision. While occasional floaters are normal, a sudden increase can be a sign of diabetic retinopathy.
As diabetic retinopathy advances, symptoms can become more severe:
- Dark or Empty Areas: You may notice dark or empty areas in your vision, indicating that the retina has been damaged.
- Impaired Color Vision: Colors may appear washed out or faded.
- Vision Loss: In advanced stages, diabetic retinopathy can lead to significant vision loss or even blindness.
If you experience any changes in your vision, it's essential to schedule an appointment with your eye doctor promptly. Early detection and management of diabetic retinopathy can help slow its progression and prevent vision loss.
What Can Be Done to Manage Diabetic Retinopathy?
How to Slow Down Its Progression
Managing diabetic retinopathy starts with controlling the underlying factors that contribute to its development and progression. This means keeping your blood sugar levels, blood pressure, and cholesterol within a healthy range. Work closely with your healthcare team to develop a comprehensive diabetes management plan that includes:
- A balanced diet
- Regular physical activity
- Medication adherence
- Stress management techniques
Did You Know? According to the National Eye Institute, people with diabetes who maintain an A1C level below 7% can reduce their risk of developing diabetic retinopathy by as much as 76%.
In addition to managing your diabetes, regular comprehensive dilated eye exams are crucial for early detection and timely treatment of diabetic retinopathy. The American Diabetes Association recommends that people with type 1 diabetes have an initial dilated eye exam within 5 years of diagnosis, while those with type 2 diabetes should have an exam at the time of diagnosis. Follow-up exams should be scheduled annually or as recommended by your eye doctor.
During these exams, your eye doctor will use special equipment to view the back of your eye and check for signs of diabetic retinopathy, such as:
- Microaneurysms
- Hemorrhages
- Hard exudates
- Cotton wool spots
Early detection allows for prompt treatment, which can slow the progression of diabetic retinopathy and help preserve your vision.
FAQ
What causes diabetic retinopathy?
Can diabetic retinopathy be prevented?
What is the first symptom of diabetic retinopathy?
How can you tell if diabetes is affecting your eyes?
Can diabetic retinopathy be improved?
What are two symptoms of early stage diabetic retinopathy?
What is the best treatment for diabetic retinopathy?
Can surgery cure diabetic retinopathy?